Itraconazole - An Antifungal Drug Effective in Colon Cancer
A Study of 5,221 Patients Showed a Major Increase in 5-Year Survival
In my 42-year career as a physician in treating thousands of patients, I have seen many afflicted with colon cancer, and none of them were told that itraconazole, a common antifungal drug, might double their survival. None of these patients were told that taking itraconazole could allow them to live longer.
However, the PubMed literature is quite clear that it can and does. That no patients are informed is a disgrace. I hope as many people as possible read this article and share it.
The medical literature has published the anticancer benefits of itraconazole for many years. Studies date back to at least 2015 when a case report was published about a patient with Stage III pancreatic cancer.
A 64-year-old male was diagnosed with non-operable Stage III pancreatic adenocarcinoma and treated with the usual platinum-based and highly toxic chemotherapy.
[By comparison, Itraconazole is FDA-approved to treat fungal infections and is considered relatively safe, although in rare cases it can produce liver toxicity, and it can interact with blood thinners to increase bleeding. Although generally safe, it should always be taken only under a physician’s supervision.]
Following treatment with cisplatin, capecitabine, and radiation, there was little response, and his tumor remained inoperable. He was therefore given palliative care including gemcitabine and erlotinib. Following this, he developed paralysis of his entire lower body due to the development of a spinal cord hemisection. He was taken to surgery for the paralysis.
Due to the chemotherapy toxicity, his white cell count dropped dangerously low. This suppressed his immune function making him vulnerable to a host of infections ranging from bacteria to fungi.
He developed disseminated histoplasmosis. It is a potentially fatal fungal infection often seen following chemotherapy in immune suppressed cancer patients.
His cancer treatments were suspended, and lifesaving measures were taken to address the histoplasmosis. He was treated with a nine-month course of itraconazole. Following this, his pancreatic cancer shrunk to the point his tumor became operable, and surgery successfully removed it.
Over the following four years, he showed no evidence of pancreatic tumor relapse. There were no metastases. The shrinkage of his pancreatic cancer was felt to be due to itraconazole.
Unfortunately, he later developed weight loss and a new primary cancer, NSCLC. Secondary lung cancers are known to be a risk following radiation therapy treatments for primary cancer.
Following this case, research in repurposing itraconazole as a cancer treatment surged. Dr. Pan Pantziarka and his ReDO Project published a review paper on itraconazole and noted multiple anticancer mechanisms of action:
Anti-angiogenic
Hedgehog pathway inhibition
Autophagy induction
Reversal of multi-drug resistance
In addition to these mechanisms, itraconazole suppresses the formation of cancer stem cells, thereby preventing or suppressing metastases. It can block or inhibit mitochondrial pathways that produce ATP - cancer’s fuel via the Warburg Effect.
Pantziarka and colleagues noted the evidence for itraconazole was strongest against the following cancers:
NSCLC
BCC
Prostate cancer
Glioblastoma
Ovarian carcinoma
Metastatic breast cancer
Pancreatic cancer
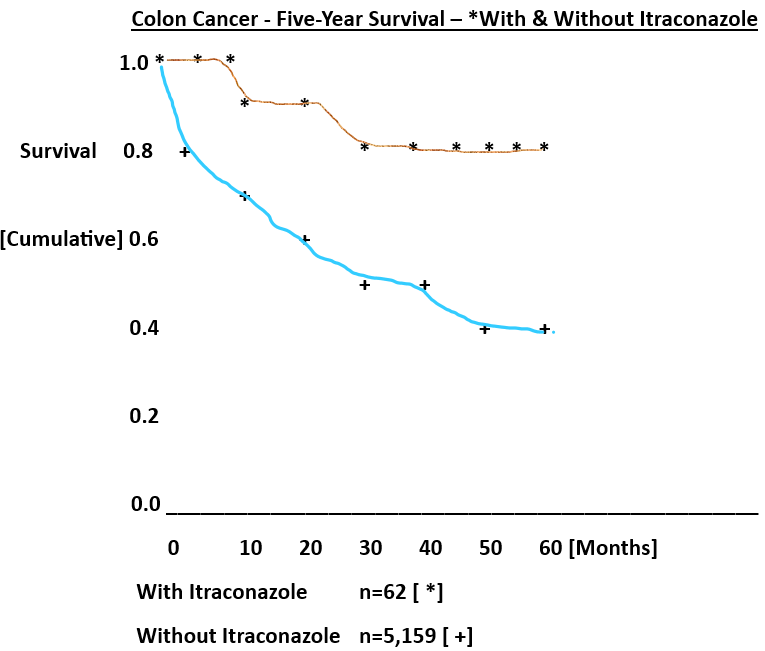
Many other studies followed, but a particularly impressive one from Taiwan retrospectively reviewed some 5000 patients with colon cancer. They looked to see which colon cancer patients had taken itraconazole and compared them with those who did not.
The results were striking, showing a remarkable and statistically significant increase in survival among those who took itraconazole.
Keep reading with a 7-day free trial
Subscribe to Repurposed Drugs: Powers & Possibilities to keep reading this post and get 7 days of free access to the full post archives.